Acne/Acne Scars
Over the past decade, advances in laser technology have allowed dermatologists to improve the appearance of scars and wrinkles and to remove benign skin growths using both ablative and non-ablative lasers
Treatment options for Acne Scars Overview
- Dermabrasion, Peels
- Erbium YAG Laser
- Subcision , excision, punching
- Dermal graft
- IPL
- Derma roller
- CROSS
- CO2 fractional Laser
- Erbium YAG fractional laser
- Rollers ( deeper) subcisions ( deeper)
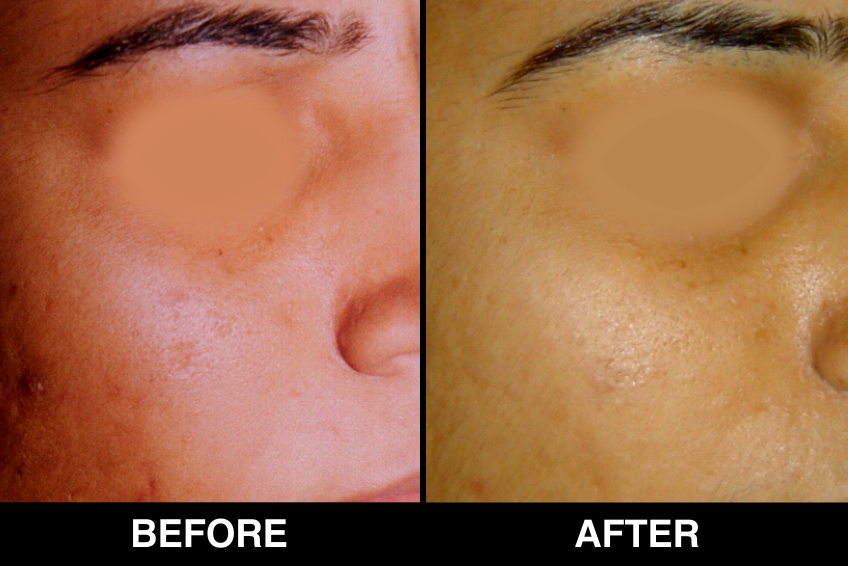
Flat Dark scars treatment options
Superficial Melanin
- Tretinoin / Hydroquinone
- Chemical Peels
- IPL
- Q switch Nd YAG
Deeper Melanin
- Q-switched Nd-YAG 1064
Red (erythematous) post acne scars treatment options
- Topical Creams
- IPL /// PDL laser treatments
Raised (Hypertrophic / keloidal scars)
- Intralesional steroid
- Intralesional 5 -FU
- Silicon sheets
- Pressure dressings
- CO2 fractional lasers
- Pulsed Dye Laser
For severe scarring Aggressive pixel
- More passes
- More density
- More fluence
- Combine procedures add 2.5 mm roller, fillers
- IV sedation
Patient selection, counseling and informed consent
As with any cosmetic procedure, proper patient selection is essential.
- History of previous laser resurfacing, dermabrasion or deep phenol peel should be noted, because these procedures could potentially delay the wound healing response due to the presence of fibrosis. Patients with a prior history of transcutaneous lower blepharoplasty and limited infraorbital elasticity may have increased risk of ectropion. When applicable, patients should be discouraged from smoking before and after surgery to reduce the risk of delayed or impaired wound healing.
- Skin to be treated should be thoroughly examined-scarring, dyschromia, rhytid formation, and skin type should be noted carefully. For patients desiring periorbital laser treatment, the eyes should be carefully examined for scleral show, lid lag, and ectropion.
- Other cutaneous disorders should also be investigated, including seborrheic keratosis, solar lentigines, actinic keratosis, acne vulgaris, and cutaneous carcinomas. The latter should be treated prior to any resurfacing procedures.
Most importantly, patients should have realistic expectations and sound reasons for deciding to undergo the cosmetic laser surgical procedure. Other cosmetic treatment options should be reviewed too so that the patient may make an informed decision.
The patient should understand that there is a postoperative healing phase with erythema and crusting that lasts for 1-2 weeks. The need to avoid sunlight during postoperative healing should be emphasized. It is worthwhile to include explicit instructions to the effect in the consent form. While CO 2 laser resurfacing is usually a one-time procedure, many patients may need repeat treatments and if the physician thinks that a second session may be needed,
Contraindications
Absolute contraindications include, active cutaneous bacterial or viral infection in the area to be treated, and ectropion (for infraorbital resurfacing).
Relative contraindications include patient history of keloid formation or hypertrophic scarring, on going ultraviolet exposure, prior radiation therapy to treatment area, and collagen vascular disease.
Caution should be taken with patients who smoke or who have a history of previous laser resurfacing, phenol chemical peel, dermabrasion, and/or transcutaneous lower blepharoplasty.
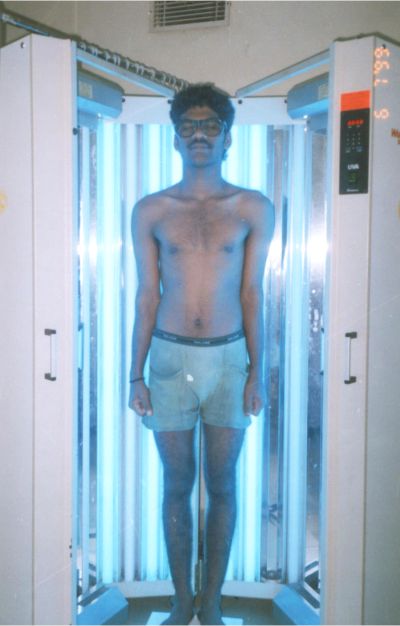
Anesthesia
For small lesions, EMLA cream applied under occlusion for 30-60 minutes is adequate. For localized areas, local infiltration with 1% lidocaine and epinephrine is usually sufficient to produce adequate anesthesia. For larger areas, such as full-face resurfacing, nerve blocks ( e.g ., supraorbital, supratrochlear, infraorbital, mental) may be needed along with local infiltration.
Postoperative care and complications
- Carbon dioxide laser resurfacing imparts a thermal injury to denuded skin. Nearly all patients encounter minor side effects ranging from postoperative pain and edema to pruritus and tightness.
- Postoperative edema (swelling) may occur, which usually subsides with cold compresses and nonsteroidal anti inflammatory drugs.
- A mild serous (watery) discharge is seen, which subsides spontaneously by the 2nd or 3rd postop day.
- Avoidance of undue sun exposure and use of broad spectrum sunscreens is mandatory.
Complications after laser resurfacing
Minor complications although frequent, are usually of minimal consequence and include milia formation, perioral dermatitis, acne and/or rosacea exacerbation, contact dermatitis, and post inflammatory hyperpigmentation. Hyperpigmentation (darkening) or erythema (redness) over the treated area is common in coloured skin and causes anxiety to patients. However, this is temporary, lasting for only about six weeks and gradually improves.
















Acne FAQ’s
Acne vulgaris is a chronic inflammatory disease of the pilosebaceous unit (hair follicles and their accompanying sebaceous glands). It can present with non inflammatory open and closed comedones and/or inflammatory papules, pustules along with pigment changes and scarring. It most commonly affects the face and to a lesser extent, back and chest.
Acne vulgaris has a mulifactorial pathogenensis, resulting from a combination of increased sebaceous gland activity with seborrhoea,abnormal follicular differentiation with increased keratinization and inflammation. Also, there is excessive growth of the bacterium Propionibacterium acnes, which is normally present on the skin.
The role of diet in acne is unclear as there is no high quality evidence to establish the link. There are studies indicating a link between a high glycaemic load diet and acne. Also, there are studies which found that milk intake increased the risk of acne.
In some cases, acne may persist into adulthood. Such types of acne include severe forms that affect the body as well as the face (which afflict males more than females) and acne associated with the menstrual cycle in women. In other cases, acne may not present itself until adulthood. Such acne is more likely to affect females than males.
That depends on many factors: your age, whether you’re male or female, how severe your acne is, and how long you’ve had it, among others. There are several options available.
Many people still believe that acne is caused by dirty skin. The truth is, washing alone will not clear up or prevent acne. Washing does, however, help remove excess surface oils and dead skin cells. Many people use all kinds of products, including alcohol-based cleansers, and scrub vigorously, only to irritate the skin further and worsen their acne. Washing the skin twice a day gently with water and a mild soap is usually all that is required. However, acne is actually caused by a variety of biologic factors that are beyond the control of washing. For that reason, you should use appropriate acne treatments for the acne.
The time for improvement depends upon the product being used, but in almost all cases it is more a matter of weeks or months instead of days. Most dermatologists would recommend the use of a medication or combination of medications daily for 4 to 8 weeks before they would change the treatment.
Look for "noncomedogenic" cosmetics and toiletries. These products have been formulated so that they will not cause acne.
Book An Appointment